- ホーム
- > 洋書
- > ドイツ書
- > Mathematics, Sciences & Technology
- > Medicine & Pharmacy
- > general survey & lexicons
Full Description
This open access book is a groundbreaking volume that creates a new field within the intersection of "global health" and "LGBTQ health" delineating specific health challenges and resiliencies. There has been increasing awareness of the importance in recognizing LGBTQ health issues and disparities. However, there is a dearth of research and scholarship that examines LGBTQ health through global and comparative perspectives. This book addresses this gap.
In the pursuit of scientific inquiry, the disciplines in public health have often emphasized reductionist perspectives that are particularized to a specific locale, municipality, or country. This book's provision of broader perspectives, cross-cutting disparities and issues, and socio-political-cultural contextualization inform the development of new research, policies, interventions, and programs. Students benefit by learning about LGBTQ health research, policies, and programs in various countries and regions. Public health researchers benefit by learning about research conducted in various countries and regions, along with understanding how research has been linked to and impacted by various policies and programs. Policymakers benefit from learning about overarching and comparative perspectives that could inform more effective policies, including those connected to multiple locations. Practitioners learn about various public health practices in multiple countries and regions that could contribute to novel and creative solutions and approaches within the respective contexts.
The nine chapters of this volume facilitate greater socio-political-cultural awareness, sensitivity, and competence; undertake an in-depth literature review of health factors and outcomes; and provide recommendations for increasing health-related capacity through development and collaborations between agencies, organizations, and institutions across countries and/or regions.
Global LGBTQ Health: Research, Policy, Practice, and Pathways is primarily intended for students and instructors in public health, medicine, nursing, other health professions, psychology, social work, LGBTQ or gender/sexuality studies, human rights, and the social sciences. The book is also a useful resource for public health researchers and practitioners, policymakers, and healthcare and social service providers.
Contents
Chapter 1. Introduction.- Chapter 2. LGBTQ Stigma.- Chapter 3. Global LGBTQ Mental Health.- Chapter 4. If You Don't Ask, You Don't Count: Elements to Consider in Understanding Global Sexual and Gender Minority Data on Non-Communicable Diseases.- Chapter 5. Sexual and Gender Minority Population's Health Burden of Five Non-Communicable Diseases: CVD, Cancer, Diabetes, Asthma, COPD.- Chapter 6. Community and Social Support.- Chapter 7. HIV/AIDS Among Sexual and Gender Minority Communities Globally.- Chapter 8. Global Epidemiology and Social Ecological Determinants of Substance Use Disparities, Consequences of Use, and Treatment Options Among Sexual and Gender Minority Populations.- Chapter 9. Victimization and Intentional Injury in Global LGBTQI Populations.
-
- 洋書
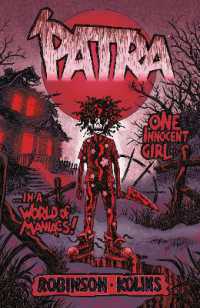
- Patra
-

- 電子書籍
- 朝5時起きが習慣になる「5時間快眠法」